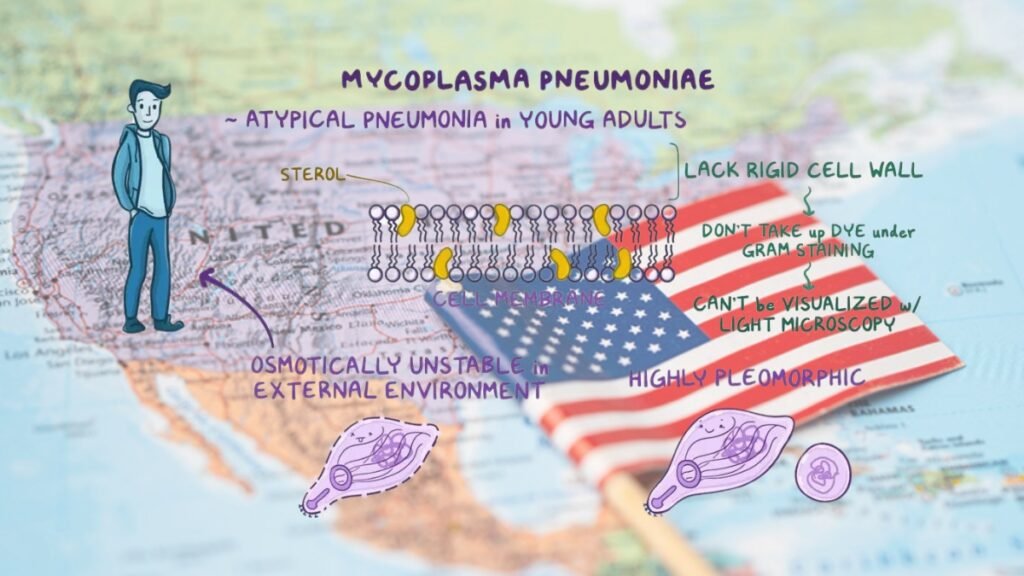
Recent data from the Centers for Disease Control and Prevention (CDC) indicate a sharp rise in Mycoplasma pneumoniae (M. pneumoniae) infections among young children, specifically those aged 2–4 years, throughout the United States. Known for causing “walking pneumonia,” this bacterial infection usually presents with mild symptoms such as a persistent cough, sore throat, and low-grade fever. However, recent cases show increased severity in some patients, causing more significant respiratory symptoms that push emergency department visits upward. This trend has garnered the attention of healthcare professionals and public health authorities alike.
Post-Pandemic Effects on Immunity and Infection Rates
One factor behind this surge may be the impact of the COVID-19 pandemic on children’s immune systems. During the pandemic, children’s exposure to common pathogens was minimized due to social distancing and lockdown measures, potentially leading to reduced immunity against respiratory infections. Now, as schools and public activities resume, children are encountering these pathogens in large numbers, with many contracting Mycoplasma pneumoniae for the first time. The CDC’s tracking data indicates that infection rates among 2–4-year-olds have risen dramatically, from 1.0% to 7.2%, while rates among children aged 5–17 have jumped from 3.6% to 7.4%.
Challenges of Antibiotic Resistance
Adding to the challenges, Mycoplasma pneumoniae infections have shown increasing resistance to macrolides, the primary class of antibiotics used to treat this infection. Although resistance levels in the United States are still relatively low, they vary significantly by region, with rates reported as high as 20% in certain areas. This resistance limits treatment options and underscores the importance of cautious antibiotic use to prevent further resistance. The CDC has ramped up surveillance to closely monitor these resistance patterns, which is critical to developing adaptive treatment protocols that ensure effective patient outcomes.
Government and CDC Initiatives for Prevention and Control
The rise in M. pneumoniae infections has prompted a series of preventive measures from health authorities and the government. The CDC has taken multiple steps to mitigate transmission and educate the public on recognizing symptoms and seeking timely medical advice:
- Enhanced Surveillance: The CDC is intensifying its surveillance efforts to monitor Mycoplasma pneumoniae infection rates and antibiotic resistance patterns across various regions. By closely tracking cases, they aim to identify outbreak clusters early, allowing for targeted public health interventions.
- Public Awareness Campaigns: Through collaborations with state health departments, the CDC is rolling out campaigns focused on educating parents, caregivers, and schools about the symptoms of Mycoplasma pneumoniae and how it spreads. They emphasize the importance of early diagnosis and proper treatment, discouraging the unnecessary use of antibiotics to reduce resistance.
- Strengthening Infection Control in Schools: The CDC has partnered with school districts to improve infection control practices within educational institutions. These include guidelines on frequent handwashing, proper ventilation, regular sanitization of classrooms, and encouraging children and staff to stay home if they exhibit symptoms of respiratory illness. This approach is critical for preventing transmission in highly populated settings where children are at increased risk.
- Encouraging Immunity-Boosting Measures: The CDC has recommended regular flu vaccinations and general immunity-boosting practices as indirect methods of reducing susceptibility to respiratory infections like Mycoplasma pneumoniae . By improving general immunity, the overall risk of severe respiratory infections can be minimized, especially in children who may have weaker immune systems due to limited exposure to pathogens during the pandemic.
- Research and Development of Alternative Treatments: Given the growing antibiotic resistance in Mycoplasma pneumoniae, the government is also supporting research to explore alternative treatments and develop new antibiotics. These initiatives aim to ensure that physicians have more effective options if resistance levels continue to rise.
- Guidance for Healthcare Providers: The CDC has issued updated guidelines for healthcare providers, advising them on the importance of differential diagnosis when treating respiratory illnesses. This guidance helps clinicians recognize M. pneumoniae infections based on symptom profiles and encourages the use of targeted antibiotics to limit resistance development.
- Hand Hygiene and Masking Recommendations: Emphasizing preventive health measures, the CDC has highlighted simple steps like hand hygiene and masking during illness as effective strategies to limit the spread of Mycoplasma pneumoniae. These guidelines are particularly targeted at high-risk groups, such as children in daycares and schools, where respiratory infections are more likely to spread.
Preventive Practices for Families and Caregivers
In addition to CDC and government efforts, families are encouraged to adopt preventive practices at home. Proper handwashing, disinfecting high-touch surfaces, and ensuring good ventilation in indoor spaces can reduce exposure to respiratory pathogens. Parents are advised to watch for symptoms such as persistent coughing, fever, and sore throat, especially if other children in the community have reported similar infections.
The resurgence of Mycoplasma pneumoniae highlights the importance of adapting to post-pandemic changes in immunity and understanding the impact of antibiotic resistance. Through proactive government action, vigilant healthcare, and public awareness, steps are being taken to mitigate the impact of this trend and protect vulnerable populations, especially young children.